


Written by Emily Cross.
20 minute read

Article reviewed by Paul Jameson, Co-Founder of Aura on May 30, 2025.
You may have heard some discussions in the news about the UK’s Assisted Dying Bill and wondered what it means for those with a terminal diagnosis and their loved ones. You may even be in the tough position of learning about the topic because yourself or someone close to you has received a terminal diagnosis, making this an issue that touches close to home.
As the bill continues to progress through parliament, understanding its key provisions, safeguards, and the ethical arguments involved is more important than ever. Whether you’re personally affected, a medical professional, or simply curious about the legislation, this article will explore the bill and its implications for patients, their families, and society as a whole.
Key takeaways:
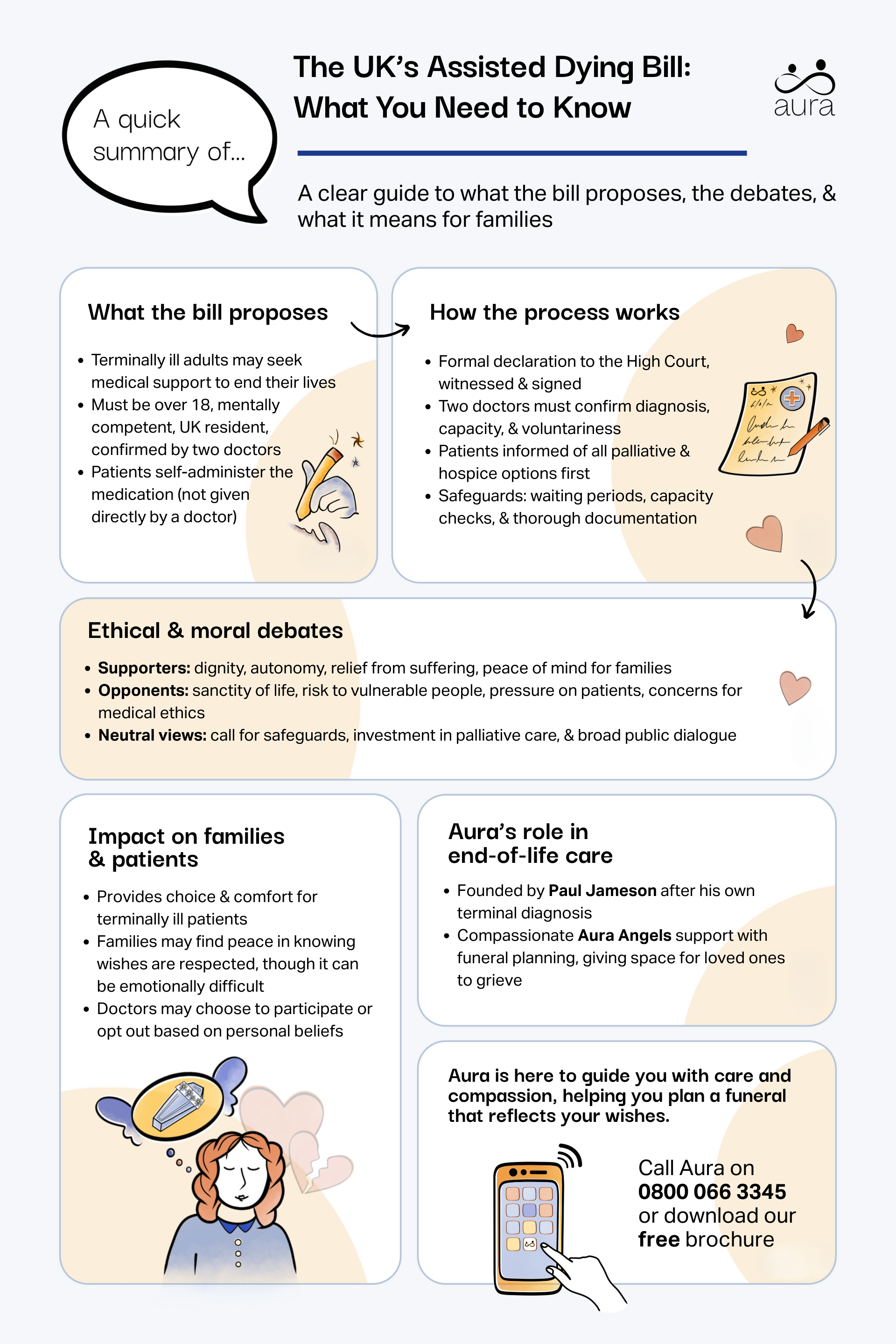
The Assisted Dying Bill, or the Terminally Ill Adults (End of Life) Bill, is a legislative proposal in England and Wales aimed at allowing terminally ill adults to seek medical assistance in ending their own lives, so long as strict criteria are met. It intends to offer people autonomy in their final moments while making sure its misuse is prevented by having robust safeguards in place.
In the UK, assisted dying, sometimes referred to as ‘assisted suicide’ or ‘medical aid in dying’, remains a contentious topic, and is fraught with moral and legal challenges. While nations like Switzerland and Canada permit assisted dying, the UK has typically prohibited it, resulting in the terminally ill travelling abroad for help, or enduring prolonged suffering at home.
Passionate voices in the conversation may lead you to think that assisted dying is the same as euthanasia; however, while they are related topics, they are not identical. We can distinguish it from euthanasia by highlighting the function of assisted dying: it enables a terminally ill patient to voluntarily end their own life, typically with a prescribed substance taken orally. This is different from euthanasia, which would entail a physician themselves actively administering a life-ending intervention. The bill focuses solely on assisted dying, and keeps it a voluntary choice for terminally ill patients.
The proposed law would apply only in England and Wales. (Health-related laws are often devolved, but assisted dying is treated as an issue of justice, which for England and Wales is decided at Westminster.)
Readers in Scotland should note that this Westminster Bill would not cover Scotland. Scotland has its own Assisted Dying Bill in progress, introduced in 2024 by MSP Liam McArthur, which is undergoing scrutiny in the Scottish Parliament. That proposal is separate and would only apply in Scotland if passed.
Currently, Northern Ireland has no similar bill being considered, and assisted dying remains illegal there (as in the rest of the UK for now). Elsewhere, the Isle of Man and Jersey have also been exploring assisted dying legislation, reflecting a broader debate across the British Isles.
The Assisted Dying Bill outlines specific eligibility and procedural requirements designed to uphold ethical and legal standards. Here are the key criteria and processes:
The bill explicitly states what requirements a person needs to meet in order to qualify for assisted dying. It applies solely to mentally competent adults aged 18 or over who have been diagnosed with a terminal illness with a life expectancy of six months or less.
The person must also have ordinarily been a resident in England and Wales for at least one year, and be registered as a patient with a general medical practice in England or Wales to qualify. The bill specifically excludes individuals whose condition is solely a mental illness or disability without a terminal prognosis, in other words, a person must be terminally ill and not just disabled or mentally ill to qualify.
“Terminally ill” is defined in the Bill as having an irreversible illness with a prognosis of around six months or less to live. This must be a progressive, incurable condition. Notably, a person won’t be considered terminally ill just because they voluntarily stop eating or drinking; eligibility hinges on the illness itself.
Patients are required to submit an application and a signed, formal declaration to the Family Division of the High Court. This declaration will state that they have a voluntary, clear, settled and informed wish to end their own life. The declaration has to be submitted using a particular document and involves multiple witnesses. It needs to be deemed to have been made voluntarily, with full understanding on the part of the applicant, and to be free from any coercion or manipulation.
It must also be signed by two doctors: an attending and an independent doctor, who have both assessed the applicant separately. They should feel wholly satisfied, without a shadow of a doubt, that the patient is terminally ill and has the capacity to make such a decision. They must feel confident that the patient has arrived at their decision voluntarily and on an informed basis.
Before countersigning a declaration, both the attending doctor and the independent doctor must ensure that the individual has been fully informed about the palliative, hospice, and other care options available to them. If they have any doubt as to the person’s capacity to make the decision, they are required to refer the person for assessment to an appropriate specialist.
There are multiple safeguards in place:
Legal protections and offences
The bill also introduces new legal protections and offences:

The Assisted Dying Bill has sparked extensive debate, reflecting deeply held beliefs on life, death, and autonomy. It is shining a bright light on the differences of opinion of UK citizens, especially when it comes to beliefs on death and funerals in religion.
Supporters argue that the bill upholds values of personal autonomy and compassion for the suffering of others. They assert that it allows those with terminal illness to avoid unnecessary pain and prolonged agony, and that it is an empathetic approach for people feeling stuck in their diagnosis.
Many believe that assisted dying lets patients die on their own terms, maintaining dignity and avoiding a potentially drawn-out, painful decline. It can spare patients the distress of losing control over their bodily functions or enduring significant dependence on others, both physically and financially.
Proponents of the bill also emphasise the psychological comfort that can come from a person being able to exercise control over their own end-of-life journey. When assisted dying is an option, it can offer significant peace of mind to everyone involved… even if they ultimately choose not to proceed with the assisted death.
Another perspective that supporters point to is that of the family members of the terminally ill person. Witnessing a loved one suffer is deeply distressing for families and friends. Assisted dying offers them a chance at a more calm, considered and planned goodbye. They are also able to employ the support and guidance of a death doula, who can assist in weaving ceremony into the day or even plan for a celebration of life. Having the option of assisted dying can have the connecting effect of opening up conversations about dying, or how to say goodbye.
Aura’s founder Paul Jameson is one such supporter of assisted dying. After being diagnosed with motor neurone disease, it’s become a passionate topic for Paul, whose impetus to start Aura was spurred by what he saw as a lacking system in the UK.
In his book Very Much Alive, Paul dedicates an entire chapter to his beliefs on assisted dying, with one section that reads:
“Recently, I asked my three children whether they would support me in a decision to end my life if my suffering, both physical and mental, became unbearable. All three said yes. It would be a win-win for everyone concerned. I wouldn’t have to suffer; and my family wouldn’t have to endure watching me do it. Ultimately, I believe, they would respect me for taking this difficult decision, for being proactive and taking control of the end of my life, just as I have throughout the rest of it.
“I love the eulogy that M delivers for James Bond at the end of No Time To Die. ‘The proper function of man is to live, not to exist. I shall not waste my days in trying to prolong them. I shall use my time.’ That sums up my attitude to life and death perfectly.”
Critics of the bill voice concerns over the sanctity of life, fearing a slippery slope towards normalising untimely death. There is also the concern that by passing an assisted dying bill, fewer resources and consideration will be granted towards end-of-life comfort measures such as palliative care. If assisted dying becomes the norm, it might shift the focus from developing better techniques and medications in favour of ending life. They feel that more weight could be placed on improving palliative and hospice care to reduce suffering without resorting to assisted dying.They argue that with better research and support, the desire for this option could be significantly reduced.
Despite the decline of religion in the UK, one of the main drivers for much of the opposition comes from religious morality. Many religious texts view life and death as under divine authority, making assisted dying morally unacceptable. For people with this outlook, human life is inherently sacred and should not be ended prematurely, regardless of the circumstances.
Opponents worry about the potential for misuse in cases of vulnerable individuals, such as the elderly, disabled, or those in financial distress. These patients in particular could feel pressured into choosing assisted dying due to familial or societal factors. Additionally, the principle of “do no harm” in medical practice is cited, with the argument that assisting in death conflicts with the role of healthcare professionals. There are concerns about eroding trust in doctors if they participate in assisted dying.
Those with a more neutral perspective consider the bill’s broader societal impact, thinking about whether or not it aligns with evolving attitudes toward end-of-life care and whether healthcare resources are adequately equipped to handle such cases. Those in the neutral camp have a more nuanced understanding of the Assisted Dying Bill, focusing on evidence, inclusivity, and careful consideration of all involved parties.
Neutral observers recognise the importance of respecting personal autonomy but highlight the need for strong safeguards to protect vulnerable individuals from coercion or misuse, such as those with dementia or other age-related cognitive conditions. They may suggest that while assisted dying could offer relief to some, it is important for the bill’s framework to ensure fairness and accessibility.
Like those in opposition, people with a more neutral outlook also have questions about whether healthcare providers are adequately trained and supported to navigate the ethical and practical challenges of assisted dying often raise. They might argue for greater investment in palliative and hospice care as complementary or alternative solutions to assisted dying. They advocate for broad public and professional discussions to ensure that any legislation reflects a wide range of views.
The Assisted Dying Bill has undergone several iterations in the UK Parliament, with passionate arguments on both sides.
The bill passed its second reading in the House of Commons on 29 November 2024 and its third reading on 20 June 2025 ,with 314 MPs voting in favour and 291 against. These votes were unwhipped, meaning MPs voted according to their conscience.
It then moved to the House of Lords, where it had its second reading in September 2025 following extensive debate. Lord Falconer is the bill’s sponsor in the Lords. However, assisted dying is not yet legal. The bill must still pass through further parliamentary stages (including committee, potential amendments, and a third reading in the Lords) and receive Royal Assent before it becomes law.
Even if passed, implementation would take time. Experts suggest that it could take up to two years post-legalisation to set up the necessary systems and oversight bodies. So, the earliest assisted dying could become available would be at least a couple of years from now.
In September 2015, MP Rob Marris introduced an Assisted Dying Bill to the Commons, but it was defeated at second reading following a four-hour debate. In October 2021, Baroness Meacher brought a bill to the Lords. It passed a second reading unopposed but ran out of time before it could progress. Earlier, in 2014, Lord Falconer also introduced a bill with similar aims, but it didn’t complete its stages before the 2015 general election.
These past efforts show how difficult and contentious it has been to change the law—but they also set the stage for the current bill’s renewed push.
Supporters such as Dignity in Dying and prominent MPs have lent their voices to the initiative, and Dame Esther Rantzen has weighed in, declaring herself an advocate for the bill. Opposition groups like Care Not Killing continue to resist its progression.
The bill’s journey reveals the intricate challenges of navigating complex moral and legal frameworks.
For terminally ill patients, the bill provides the opportunity for a legal and dignified option to end their suffering. It can give them comfort knowing they have the ability to access this type of support without needing to travel to another country during an already challenging time, and provide space to think about planning their own funerals or making other arrangements. Families may find solace in knowing their loved ones’ wishes are respected, but could also face emotional challenges in accepting such decisions.
Relatives and friends would be shielded from legal repercussions when supporting a loved one’s choice under the proposed law.
The bill introduces significant changes for healthcare practitioners. Doctors would have the right to opt in or out of participating based on personal beliefs… However, it raises questions about their role in facilitating death and the emotional burden this responsibility may impose should they choose to support it.
The UK’s Assisted Dying Bill draws inspiration from countries where such practices are legal. For example:
In studying these systems, the UK can learn valuable lessons on implementing balanced and tested approaches.
The UK’s Assisted Dying Bill incorporates several protective measures to safeguard vulnerable individuals from coercion, undue influence, or potential abuse or manipulation. These measures ensure that only those who genuinely meet the criteria and make an informed, voluntary choice can access assisted dying. Key protections include independent medical assessments by qualified medical professionals, mental capacity evaluations, a mandatory waiting period, witnessed consent, information about alternatives such as hospice and palliative care, oversight and monitoring, and professional safeguards such as an opt-out of participation.
These protections are designed to make sure that the autonomy of terminally ill individuals is upheld, while preventing exploitation or harm to vulnerable populations.
Assisted dying requires patients to self-administer life-ending medication, while euthanasia involves direct action by a doctor. Though some countries have legalised euthanasia, the proposed UK bill strictly addresses assisted dying.
For the bill to become law, it must pass through parliamentary debates, receive royal assent, and gain public support. Legal and ethical concerns remain significant obstacles to its enactment.
Aura was founded by Paul Jameson, following his diagnosis with motor neurone disease and motivated by his experience navigating end-of-life care. He didn’t want his family to struggle with unorganised affairs and an impersonal funeral. His aim was to leave a lasting legacy, one that honoured his spirited and joyful outlook on life.
He was able to turn his confrontation with his own mortality into a positive with Aura, where we strive to offer a level of service that Paul would want for himself and his own family.
We provide unique services such as a pre-paid direct cremation plans, for both attended and unattended cremation services, to meet the needs of those looking to do things in their own way. Our plans allow you to take care of the costs and details of your funeral ahead of time, so your family will have the space to grieve without worrying about finances or the stresses of planning. Aura is regulated by the Financial Conduct Authority (FCA), and our plans are protected by the Financial Services Compensation Scheme (FSCS). You can rest assured that, when you purchase a prepaid funeral plan from Aura, your money is secure.
Many people opt to sort out details ahead of time and compare funeral plans; choosing the right plan is a deeply personal decision. Whatever you decide, it is important to recognise that though we can’t plan for every eventuality, we do have a certain amount of control over our end-of-life decisions in the UK.
If you’re looking for support making funeral arrangements, our compassionate angel team are here to help.


The Assisted Dying Bill proposes to allow terminally ill adults in England and Wales—with a life expectancy of six months or less—to legally end their life with medical assistance, under strict eligibility and procedural safeguards.
To qualify, a person must:
Be aged 18 or over
Have mental capacity to make the decision
Be diagnosed with a terminal illness (six months or less to live)
Be ordinarily resident in England or Wales
Be registered with a GP in England or Wales
No.
Assisted dying requires the person to self-administer the life-ending medication.
Euthanasia involves a doctor actively ending the person’s life.
The UK bill focuses on assisted dying only.
No, euthanasia is illegal in the UK. It’s considered a criminal offence. The Assisted Dying Bill currently in Parliament does not legalise euthanasia — it only allows terminally ill adults to self-administer life-ending medication under strict safeguards.
The person submits a formal, witnessed declaration to the High Court.
Two doctors (attending and independent) assess and approve the request.
Safeguards like waiting periods and mental capacity evaluations are applied.
The person self-administers the prescribed medication if they choose to proceed.
Two independent doctors must confirm eligibility and capacity.
The individual must be informed of all care alternatives (e.g. hospice).
The request must be voluntary, with no external pressure.
Witnessed consent is required.
A mandatory waiting period allows time for reflection.
Mental health evaluations are mandated if there’s any doubt about capacity.
Oversight is provided by the courts and healthcare bodies.
Supporters believe it upholds personal autonomy, offers compassionate relief from suffering, and provides terminally ill people with choice, control, and dignity in their final days.
Opponents worry about:
Potential pressure on vulnerable individuals
The erosion of medical ethics (e.g. “do no harm”)
Religious and moral objections
A possible shift away from investing in palliative care
The risk of a “slippery slope” toward broader criteria
Doctors would have the legal right to opt in or out of participation. Those who choose to support patients through assisted dying must follow the strict protocols laid out in the bill. Emotional, ethical, and professional implications are being debated.
If passed, the UK would join a growing number of countries (e.g. Canada, Switzerland, parts of the US) in legalising assisted dying under specific, regulated conditions. The bill would still need further readings and royal assent before becoming law.
If it became law, assisted dying could involve doctors and healthcare systems, so the NHS could have a role. There is however, no confirmed NHS assisted dying service planned yet.